One in every two Australian women is estimated to have a common chronic health condition.
One in two. That's 49 percent of women.
Meaning? If you don't suffer from a chronic health condition, chances are the woman sitting beside you does.
Because here's the thing – you don't have to *look* sick to be battling an illness.
From endometriosis to mental health illnesses, back issues and diabetes, the umbrella term ‘chronic condition’ offers up a broad range of health issues – often complex and non-communicable conditions that are scattered across a wide spectrum of illnesses.
Watch: Things guys need to know about endometriosis. Post continues below.
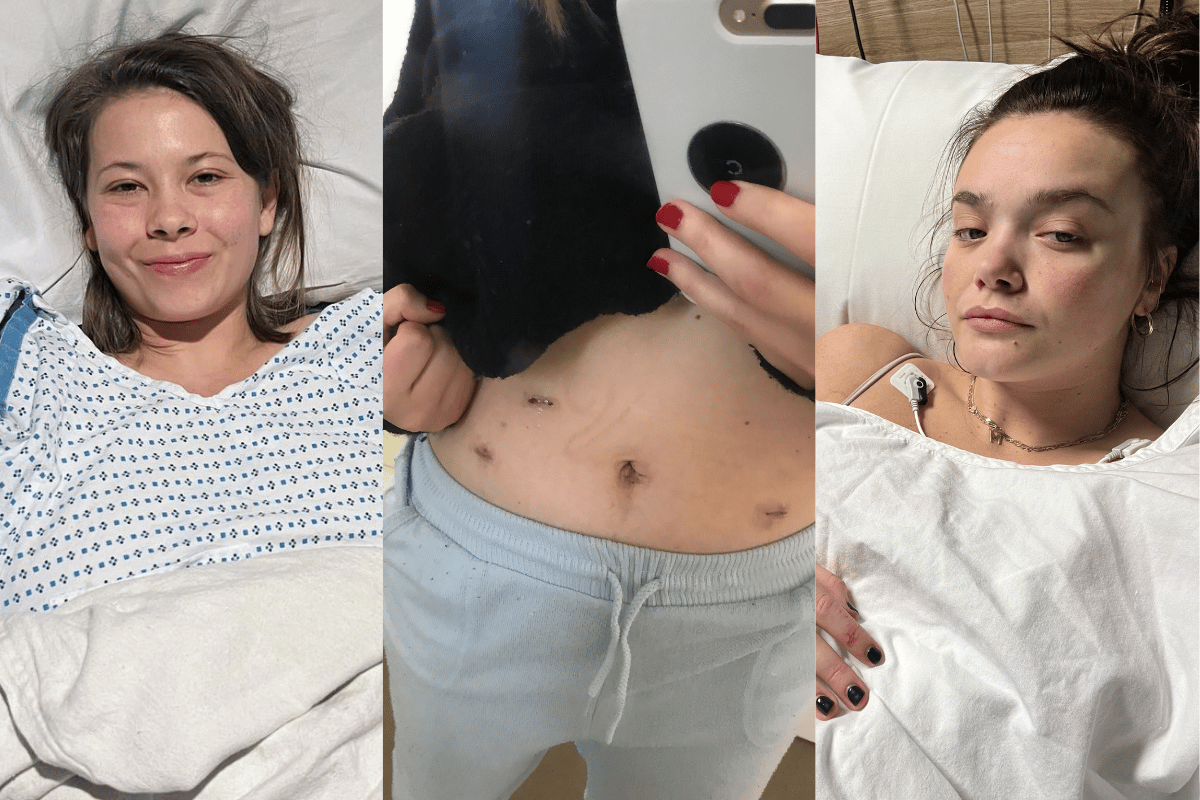
Many celebrities have shared their own experiences with invisible illness, including Bindi Irwin, who has opened up about her ongoing battle with endometriosis in the past.
The 25-year-old shared that she was "trying to remain a positive person and hide the pain" but decided to share her journey to help other women in pain.
She wrote: "For 10 years I’ve struggled with insurmountable fatigue, pain and nausea," she wrote alongside a photo of herself in a hospital bed.










Top Comments